More Information
Submitted: 10 April 2020 | Approved: 27 April 2020 | Published: 28 April 2020
How to cite this article: Baltasar A. Obesity Surgery in Spain. New Insights Obes Gene Beyond. 2020; 4: 013-021.
DOI: 10.29328/journal.niogb.1001013
ORCiD: orcid.org/0000-0003-2964-8161
Copyright License: © 2020 Baltasar A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Morbid obesity; Obesity surgery; Bariatric surgery SECO
Obesity Surgery in Spain
Aniceto Baltasar*
Spain
*Address for Correspondence: Aniceto Baltasar. Alcoy, Alicante, Spain, Tel: +34 616 231 021; Email: [email protected]; [email protected]
Obesity or bariatric surgery, from the Greek bari = weight and iatrein = cure) treats obesity and began in Spain in 1972. Its greatest development occurs after the foundation of SECO (Spanish Society of Obesity Surgery) in 1997. The purpose of this work is to reflect the changes that have occurred in these 47 years.
Obesity is a multifactorial epidemic disease of environmental origin that affects subjects of all countries and whose origin is not in the stomach or intestines. Surgical treatment represents a unique case of surgery for operating healthy organs, which are not the cause of the disease and do not improve after the operation.
Kremen and Linner [1] and Varco and Buchwald teams of in Minneapolis, MN began the intestinal deviation (ID) of malabsorption in 1954. Payne [2] and Scott [3] developed these ID techniques in the 1960s leaving only 14- 4 inches (35 -10 cm) as an absorption zone and were abandoned in the 1970s due to its serious metabolic (malnutrition) and liver complications (liver failure).
To review the historical process on management by bariatric surgery in Spain in the last 47 years.
Historical note
Córdoba (Qurtuba in Arabic) was the most civilized city in Europe in the 10th century. Andalusia housed the most famous doctors of the Middle Ages, Averroes (1126-1198) and Maimonides (1135-1204).
Sancho “the fat”, king of León 956-958, was deposed due to his massive obesity. He found security in Pamplona, in the Kingdom of Navarra, 400 km from León, where his grandmother, Queen Toda, ruled. Toda’s goal was to regain the kingdom of León for his grandson, but this was impossible unless Sancho el Gordo lost his enormous excess weight.
Hasdai ibn Shaprut was a famous Jewish doctor in the court of Abdurrahman III of Cordoba. He traveled to Pamplona to evaluate Sancho’s super-super-obesity and decided that he would only treat Sancho if he arrived in Córdoba.
The 800 km trip was a terrible experience because Sancho could not ride a horse or a carriage. He remained semi-conscious for most of the trip and was in a special canvas shop, designed by Hasdai, between four mules. The queen, Toda (aunt of Abdurrahman III), Garcia (his son, the king of Navarra) and Sancho lived in Córdoba for 6 months, during the time the treatment lasted.
The treatment consisted of suturing Sancho’s lips and feeding him only with a straw. Sancho lost half of his weight and returned riding a horse to León and regained his kingdom in 959. This is the 1st published worldwide experience on the surgical treatment of obesity. Baltasar (AB) [4].
First spanish ID experience
Prof. Sebastián García Díaz [5] of Seville (Figure 1a), Spain carried out the first Scott-type jejune ileal diversion (JID) at the Virgen Macarena Hospital on 19.11.1973.
Figure 1: S. García R. Mason N. Scopinaro
He started this mal absorptive surgery with 12 cases [6-7] and then published 20 more, as well as the 1st bariatric workin English by a Spanish author [8] in 1981. His work went unnoticed for 40 years until we rescued them in 2013 [9].
In 1964 Mason (Figure 1b) [10] began gastric bypass (GBP). It was a total change in strategy with restrictive surgery (reducing food intake). It was a total change in strategy, and the 1st bariatric revolution. Capella [11,12] with 148 patients in the USA, Álvarez-Cordero [13,14] with 452 patients in MX (both honorary members of SECO since the 1st Meeting), Fobi [15,16] with 576 patients and Garrido [17] in BR 1st book of bariatric surgery in Portuguese and they have performed in the “Garrido Institute” [18] with 10 surgeons more than 22,000 cases (+ of 1,200 cases/year) and since the 70s they are the world leaders in this technique. AB [19] made on 17/7/1977 the 1st RYGBP Mason-type in Spain.
Scopinaro (Figure 1c) [20], a tireless researcher and clinician, initiated experimental and clinical gastrectomy with biliopancreatic diversion (DBP) in 1976. He is the leader and “father of European bariatric surgery” and participated in multiple conferences and publications. The operation combines a gastrectomy technique plus DBP as it is the most effective for treating obesity [21,22]. He is an honorary member of SECO and the only foreign winner of the Outstanding Achievement Award (OAAW), of the American Association of Metabolic and Bariatric Surgery (ASMBS). And he participated in IFSO-SECO Salamanca-2003 and Madrid-2019.
The DBP became an extremely popular technique in Spain. Larrad and Sánchez [23-26] published extensively on their own modification and others used this technique in Zaragoza [27-30] and Santander [31,32].
Mason [33] “father of bariatric surgery” published in 1982 vertical banded gastroplasty (VBG) and was the 2nd great revolution in BS by allowing many surgeons to do bariatric surgery. AB [30] presented at RTVE-1984 an operation of VBG, the 1st Spanish documentary, on obesity surgery in a man with BMI-52. Laporte [34] published the 1st Spanish VBG experience with 9 cases.
AB [35] broadcasted from Alcoy in 02.06.1986 the 1st Spanish documentary on RTVE as a VBG obesity surgery in Spain in a man with BMI-52.
Re-opening of the vertical stapling line was a serious disadvantage of the VBG because it cancels the restrictive effect of the operation. AB [36] in 1989 described the stapling of the gastric tube and complete division between the gastric tube and the rest of the stomach and did not have a single recanalization in 100 cases. Andreo [37] described the typical reservoir as a “peanut” radiological deformity of the VBG.
Many Spanish surgeons performed the VBG operation [38-40]. AB [42] published the 1st 100 cases in 1990 with excellent results, but ... 5 years later he reviewed the same patients and described it as “a frustrated hope” [42,43]. Two years later, this technique was abandoned.
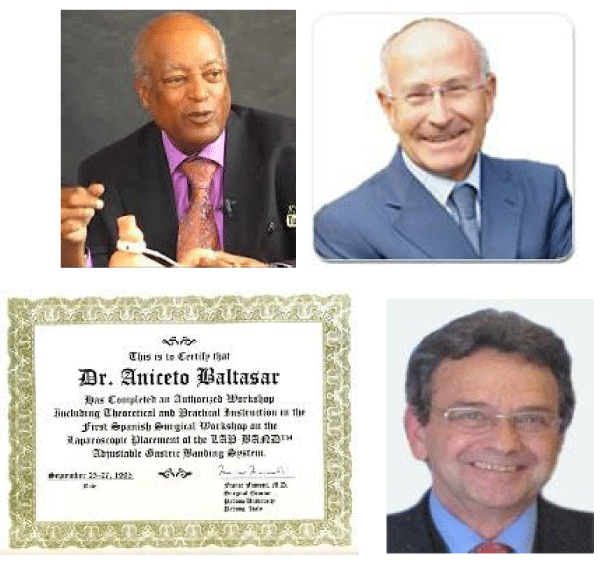
Belachew (Figure 2a) [44,45] started in Belgium on 1/9/1993 the use of laparoscopy with the 1st Laparoscopic Adjustable Band (LAB) operation. It was the 3rd revolution in bariatrics since it allows operations without opening the abdomen. Laparoscopy changed the way of doing surgery s but in all general surgery since being repetitive in bariatrics and performed in healthy organs, represented the greatest advance in all surgery of the 21st century.
Figure 2: a) M. Belachew, b) F. Favretti 1t GVAL española. “La Paz” Madrid. 1995 C. Masdevall.
Favretti [46] performed on September 27, 1995 the 1st LGB operation in Spain at the “La Paz” Hospital in Madrid (Figure 2b) with the assistance of Masdevall / AB.
Carbajo [47] in 1986 published the 1st 12 LGBs in Spain and Alastrué [48] compared the results of VBG with LGB. More than 650,000 LGBs were performed worldwide and then the technique was abandoned due to poor long-term results.
In the 1990s, the American Bariatric Surgery Society [ASBS] was the 1st national bariatric society created by Edward Mason on June 3, 1983 in Iowa City, IO [49], the city where I worked all his life. Deitel (Figure 3a) started Obesity Surgery, as the first magazine on obesity in 1990 [50].
Figure 3: a) M. Deitel, b) SECO Anagramas. SECO-1976. SECO-2015
The International Federation of Surgery for Obesity (IFSO) was founded in 1995 and so were the standards for reporting results [51].
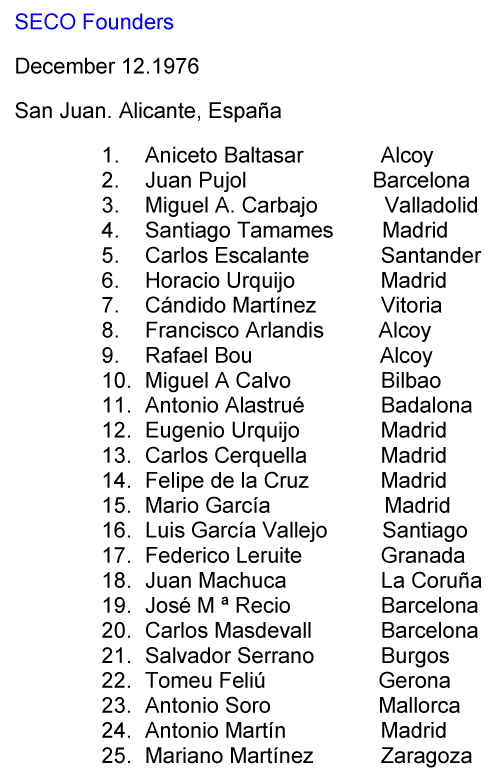
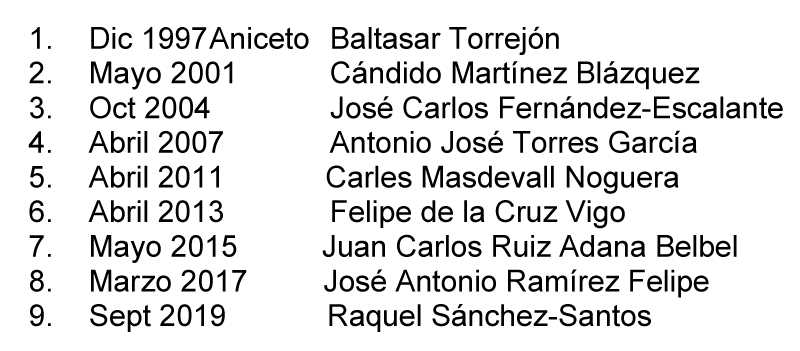
The Spanish Society of Obesity Surgery (SECO) was founded in Perez Mateos Residence, San Juan, Alicante by 26 surgeons on December 12, 1976 (Figures 3b, 4 and 5). SECO members have been continually active in publishing their works (Figures 6,7) and books (Figure 8).
Figure 4: SECO Founders.
Figure 5: List President of SECO.
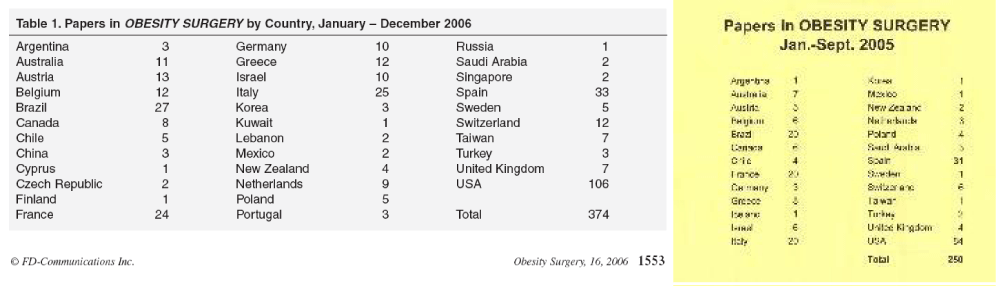
Figure 6: SECO Publications in Obes Surg. 2005-6.
Figure 7: Publicaciones de SECO en SOARD 2014.
Figure 8: Libros publicados por miembros de SECO. AB. 2000, C. Martínez, De la Cruz on DG, Caballero on diabetes.
SECO joined IFSO in 1998 and AB was President of IFSO-2002 and organized and chaired IFSO-Salamanca-2003. Dr. A. Torres was the 2nd Spanish President of IFSO and organized IFSO-2019-Madrid, the largest bariatric meeting in the world. Spain is the 2nd country to organize this congress twice.
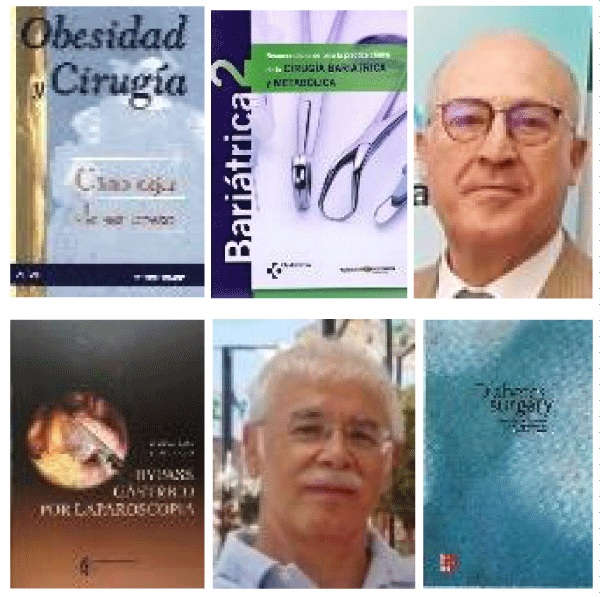
Wittgrove (Figure 9b) and Clark (Figure 9c) on October 27, 2003 [52-54] took the most significant step in performing the 1st laparoscopic gastric bypass (LGBP in San Diego. This is the 4rd revolution of the BS. AB was the 1st visitor to San Diego in September 2007. Wittgrove [55] abandoned to use the huge circular port # 33 to pass the circular stapler, under our proposal and not using that trocar and that was an especially important step.
Figure 9: LGBP. a) A. Wittgrove, b) W. Clark.
AB [56] performed the 1st LGBP in Spain on 1.14.1997 and presented it [57] in Bruges IFSO-1998 as the 1st European to report it on video. Serra [58] published in 1999 the 1st world hernia after LGBP. Higa [59] fortunately made the 1st LGBP with manual sutures.
AB [60] published the 1st book in Spanish on BS in 2000 (Figure 8a). Martínez [61] of Vitoria (Figure 8b) published a bilingual book of BS (Spanish and Basque) in 2001. De la Cruz [62] published (Figure 8c) in 2006 the 1st Spanish book on LGBP and performed the 1st surgicalsession in León. García-Caballero [63] published an English book on diabetes surgery ((Figure 8d).
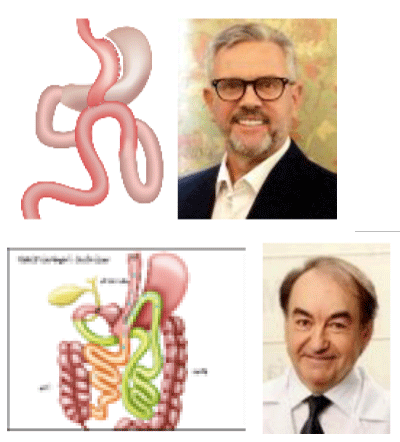
Hess [64] and Marceau [65] (Figure 10a) initiated the Duodenal Switch (DS) in 1988, as a VG plus DBP and AB [66] did it first 3.17.1994. The CD is an aggressive mixed technique of reduction in food intake and absorption.
Figure 10: Duodenal Switch. Anagram, DS draw, AB/Hess/Marceau 1996. M. Gagner.
Ren/Gagner [67] make the 1st worldwide LDS in October 1999 and AB the 5.10.2000 [68] the 1st LDS in Europe. (Figure 10c). This difficult and controversial technique of LDS by “Switchers” surgeons is rarely used today, in less than 1%. AB [69,70] had a mortality of 0.4% with LDS in 950 patients and believes that is the most effective technique to lose weight.
There have been many technical variations in laparoscopy. In general, all viscera division is done with automatic sutures. The joints (= anastomosis) are performed with automatic or manual sutures. We start the gastrectomy at the pylorus and suture the anterior and posterior gastric serosa, covering the staples with omentum, to avoid gastric tube rotation and leaks, with the sliding and self-blocking point of Serra-Baltasar [71-73]. SECO members have been very active publishing on OS and on SOARD.
SECO members were active in the first years of OS and SOARD ((Figure 6a,b)). Spain was the 2nd country with the largest number of publications, after the USA in 2005 and 2006 and in 2013 it was the 5th country with the highest number of publications in SOARD (Figure 7).
Among the founding members of SECO there has been a high volume of literature (Alcoy-124, Carbajo-76, Belvitge-38, Alastrué-30, Martín-Duce-27, Martínez C.-22, Ballesta-9, Zaragoza-5). In 2003, SECO made the Salamanca Declaration on CO [75] who gave advice on good practices in the specialty.
Laparoscopic Sleeve-forming Gastrectomy (LSFG), the restrictive part of DS, was described by several authors, in 2005. AB’s article on LSFG [75] is, according to Ahmad [76], the 61st most cited article in bariatric literature. Angrisani [77] states that the LSFG is the most performed operation in the world.
Rutledge (Figure 11a,b) described 1,274 cases of one anastomosis gastric bypass of (OAGB) in 2001 [78] and Spanish authors have developed two popular techniques. Carbajo [79] (Figure 11c-d) has since 2004 made the reservoir of less curvature without gastric resection, a GBP with lateral diversion to an intestinal loop. He presented more than 3,500 cases at the 1919 World Congress in Valladolid and today is the fastest growing technique in the world.
Figure 11: OAGP, R. Rutledge, OAGBP, MA. Carbajo.
Sánchez-Pernaute (Figure 12a) and Torres (Figure 12b) [80] from Madrid Clinic Hospital, described in 2005 the SADI (Single Anastomosis Duodenal-ileal), a type of single-anastomosis DS. There is gastric resection in the form of SFG and DBP is performed from duodenum to jejunum (D1). The operation is already extremely popular worldwide.
Figure 12: A. Sánchez, SADI, A. Torres.
Bellvitge hospital in Barcelona has organized 16 consecutive bariatric courses by the BS department and Torres/Sánchez another 16 annual courses at the Clinical Hospital of Madrid.
SECO members have participated in numerous local, regional, national, and international meetings and congresses, especially Latin Americans where SECO has always been very well received. In May 1998 AB organized the 1st Symposium at the meeting of the prestigious course of Prof. Moreno González, with Drs. Cowan, Fobi, Scopinaro, Clark and F. de la Cruz.
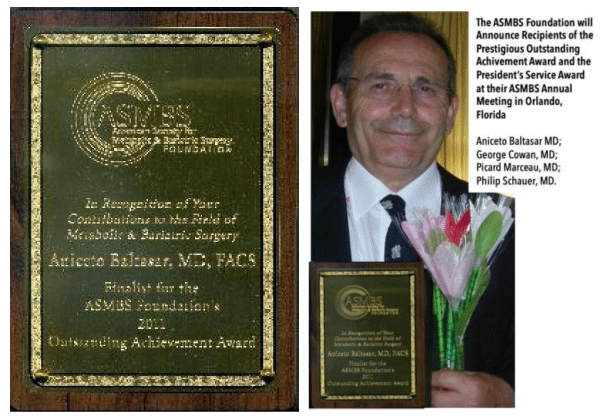
In 2003, AB opened the Spring Meeting in NY and fall in Chicago with two keynote lectures at the American Congress of Surgery on CD. AB was nominated as a finalist and received the IFSO-Lifetime Membership Award in June 2011 and was a finalist in the prestigious ASMBS-Outstanding Achievement Award at the ASMBS meeting in Orlando, Florida (Figure 13).
Figure 13: AB - 2011-AMSBS-OAAW.
In 2009, Scopinaro, Melissas, Fried and AB [81] created the IFSO European Chapter of the Centers of Excellence Program (ECEP). Currently, only three Spanish centers and surgeons use this prestigious quality control program.
We founded [82] BMI-Latina Journal (Bariatric and Metabolic Iberoamerican) in 2011 www.bmilatina.com. An online magazine published in Spanish, English and Portuguese and has been adopted by SECO in 2015 and can play a valuable role in the active societies that speaks Spanish and Portuguese. Doctors Carbajo M, Torres A and AB are honorary members of the bariatric societies of Portugal, Argentina, and Brazil.
SECO has since 2014 have an online SECO-Campus a training program in its 5th edition where many surgeons and nurses receive courses: 1) 5 Emergency courses in BS - 950 participants; 2) 3 Bariatric nursing courses - with 200 participants; 3) Family doctors - 250 participants. That is today the jewel of SECO. There are courses of experimental surgery and live surgery and programs of supervised stay in teaching centers and advanced BS courses, as the teaching online of the 21st century. https://www.campusseco.org
AB trained 72 surgeons from several countries during weekly periods of bariatric surgery. We participated in 16 live surgeries broadcast on TV in Spain. AB performed 1st VBG in 1988 in Málaga, Coimbra the 1st VBG in 1992 and LGBP in 2005. He made the 1st ODS in Sao Paulo at Portuguesa Clinic in 1999, and the 1st LDS in Itajai, SC in 2003. 1st LDS in BS as in 2001. 1st LDS in Jerusalem in 2008. 1st GVL in 2002 in Forde and 1st LDS in Tonsberg Norway in 2006, and the 1st LDS in Ahmadabad, India. An LDS [84] film got the 2º Award in IFSO-Sao Paulo 2002.
Diabetes surgery
Part of the BS is dedicated to diabetes as metabolic surgery. AB [84] publishes the 1st intervention in 2004 with a BPD-without-SFG.
Resa and Solano [85] describe 65 cases of gastro-ileal shunt as the simplest, fastest and safest technique to treat obesity. And then Resa [86] again publishes 1512 more cases. Alhambra [87], Vidal [88], Vilarrasa [89], García [90], Cruz [91] and Torres [92] have published on the same subject.
Laparoscopic BS in children and adolescents (ABS)
BS is increasingly used in children. Baltasar [93] published the first national SFG of ABS in 2004 about a 10-year-old boy with excellent results 10 years later [94].
Carbajo [95] has a case with 5 years of follow-up and then in 2019 again [96] reports the most extensive experience in ABS with 39 patients treated with OAGBP and excellent results.
Vilallonga [97] (Figure 14b) reports that the overweight rate in children aged 4 to 24 has increased by approximately 10% in the last 20 years. It is estimated that today, 20% of boys and adolescents and 15% of girls are overweight.
Robotics BS
Cadiere and Favretti performed the first robotic bariatric operation in the world at a distance in 1998. Blázquez performed the first 12 Spanish robotic bariatric surgeries in Vitoria-2013. Vilallonga is the 1st accredited robotic surgeon in Spain and Fort [98] since 2010 at the Vall d ´Hebron Hospital in Barcelona develop robotic surgery and performed more than 540 cases with the da Vinci surgical system (Figure 14a) Surgical System® (Intuitive Surgical, Sunnyvale, CA) at the beginning with GV and they robotic DG.
Morales [98] (Figure 14c) performs in Seville the complex single-port surgery since 2012 and today leads the European surgery [99].
Lacy (Figure 14d)] started AIS-Channel as a pioneer online television broadcast worldwide and performed the first BS remote operation by G5 cell phone from the Clinical Hospital of Barcelona on 4.14.2019 at the WORLD-VIDEO Forum Barcelona-2019.
Figure 14: Da Vinci, R. Vilallonga, S. Morales, A. Lacy.
There has been an international recognition in SECO members. The biography of the members of the Spanish society [100-104] has been published in Obes Surg.
Surgeries performed in Spain 2018
1st Surgery: 5,952; 2nd revision: 343:
Complications: DGL-3.7% and GVL-3.6%; DGL-Leaks-1.2%, Bleeding-2.3%, TEP-0.1% Re-op-2.3% Exitus-0.1% and in GVL-Leaks-1.5%, Hemorrhages-1.9% TEP-0.1% 2.1% Deaths-0.1%. An extraordinary good result!
Private centers report multiple operations over the years with different techniques: Valladolid-4,255, Teknon-3,000, De la Cruz-2,493, Zaragoza-2,649, Alcoy-1,729.
We have collaborated to clarify errors and published the correct terms on Wikipedia in GVL [105] https://es.wikipedia.org/wiki/Gastrectom%C3%ADa_vertical_laparosc%C3%B3pica and on DS [106] https://es.wikipedia.org/wiki/Cruce_duodenal.
Report complications
We should publish all serious complications, such as malnutrition [107], leaks [108-110], total gastrectomy [111], liver failure [112-114], stapling of the NG tube [115], tracheotomy of emergency [116] and errors such as Journal of Negative of Non-Positive Results (JNNPR) [117], since you are more likely to learn from negative results than positive ones.
The BS is performed in public centers in all regions of Spain with exceptionally low leakage rates and complications. But ... it is still not done on an outpatient basis.
Fast track surgery
If OM is an epidemic pathology and BS is the best solution, it should be accessible to more subjects. There is a good surgery system without hospitalization. Many centers are now using this technique since the cost is much lower and the security is similar.
We visited Duncan [118] who performs ambulatory CO, and this will be the 4th great bariatric revolution. They work two independent teams: Team A uses at the same time 2 operating rooms, 2 nurses in anesthesia (one per room), 2 scrub nurses and an operating room technician as an assistant. Operating times are close to 22´. The surgeon and assistant go to OR-2 with the patient already anesthetized. They change gowns and gloves and treat 5 patients in total in the morning session. In the evening, surgeon B operates while team A makes the consultations. In total 10 patients per day. 50 cases per week, 2,2000 cases per year. Not overnight stay. All patients in the morning are discharged before 2 pm. The cost of the intervention was reduced about 50%.
AGB: Adjustable Gastric Band; VBG: Vertical Banded Gastroplasty; GBP: Gastric Bypass; OAGP: One Anastomose Gastric bypass; BPD: Bilio-pancreatic Diversion; ID: Intestinal Diversion; DS: Duodenal Switch; SADI: Single Anastomose Duodenal Ileal; SFG: Sleeve- forming Gastrectomy; ABS: Adolescent Bariatric Surgery; REV: Revision surgery; MO: Morbid Obesity; WL: Weight loss; %EWL: % Excess Weight Loss; BMI-EBM: % Expected Weight loss; Add L if laparoscopic
- Kremen AJ, Linner JH, Nelson CH. An experimental evaluation of the nutritional importance of proximal and Distal small intestine. Ann Surg. 1954; 140: 439-448. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/13198079
- Payne JH, de Wind L, Schab CE, Kern WH. Surgical treatment of morbid obesity. Sixteen years of experience. Arch Surg. 1973; 106:4 31-437. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/4696715
- Scott HW, Law DH, Sandstead H, Lanier VC Jr, Younger RK. Jejunoileal shunt in surgical treatment of morbid obesity. Ann Surg.1971; 171: 770-781. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/5445664
- Baltasar A. More than 1,000 years ago, Sancho the fat lost his Kingdom. Obes Surg. 2004; 14: 1138. Book Angeles de Irisari. “The Queen’s Trip”. "El viaje de la reina". 2002. Hace más de 1.000 años Sancho El Craso perdió su reino. Entre colegas.2013.
- García Díaz S. Indicaciones del tratamiento quirúrgico en la obesidad mórbida. Rev. Quir. Española 1975; 2:165-172.
- García Díaz S, Pera C, Loscertales J. Trabajos originales. Estado actual del tratamiento de cirugía de la obesidad. Rev Esp Enf del Ap. Digestivo. 1977; 51:1-25.
- García Díaz S, Pera C, Loscertales J. Avances en cirugía. Barcelona. Editorial Salvat. 1979; 209-224.
- García Díaz S, García G. Medical and surgical indications for treatment of morbid obesity. World J Surg. 1981; 5:795-799. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/7342473
- Baltasar A, Domínguez-Adame E. Inicios de la cirugía bariátrica y metabólica en España. Cir Esp. 2013; 91:407-416.
- Mason EE, Ito C. Gastric bypass in obesity. Surg Clin North Am. 1967; 47:1345-1351. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/6073761
- Capella R, Capella J, Mandac H. Vertical Banded Gastroplasty-Gastric Bypass: preliminary report. Obes Surg. 1991; 1: 389-395. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10775940
- Capella R. Biography. Obes Surg. 2017; 27: 1129–1130.
- Álvarez-Cordero R, Aragon V. Post-operative Complications in a Series of Gastric Bypass Patients. Obes Surg. 1992; 2: 87-89. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10765170
- Álvarez-Cordero R. Biography. Obes Surg. 2016; 26: 1997–1998.
- Fobi M. Why silastic ring vertical banded gastric bypass for treatment of obesity? Obes Surg. 1991; 1: 423-426. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10775946
- Fobi M. Biography. Obes Surg. 2016; 26:243–244.
- Garrido A. “Cirurgia da Obesidade”. Editor y autor de vários capítulos. São Paulo. Editora Atheneu, 2002.
- Garrido AB. Biography. Obes Surg. 2017; 27:1399–1400.
- Baltasar A, Del Río J, Bengochea A. Baipás gástrico en la obesidad mórbida. Revista clínica española. 1980; 157: 395-399.
- Scopinaro N, Gianetta E, Civalleri D, et al. Biliopancreatic bypass for obesity: II. Initial experience in man. Br J Surg. 1979; 66: 619-620. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/497645
- Scopinaro N. Why the Operation I Prefer is Biliopancreatic Diversion (BPD). Obes Surg. 1991; 1:307-309. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10775931
- Sánchez C, Larrad N. Analysis of Weight Loss with the Biliopancreatic Diversion of Larrad: Absolute Failures or Relative Successes? Obes Surg. 2002; 12: 249-252. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11975222
- Larrad A, Sánchez C. Quality indicators in bariatric surgery and criteria for long-term success. Cir Esp. 2004; 75:301-304.
- Larrad Jiménez A, Sánchez Cabezudo C, de Quadros Borrajo PP, Ramos García I, Moreno Esteban B, et al. Course of Metabolic Syndrome following the Biliopancreatic Diversion of Larrad. Obes Surg. 2007; 17: 202-210. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15527630
- Larrad-Jiménez A, Díaz-Guerra CS, de Cuadros Borrajo P, Lesmes IB, Esteban BM. Short-, Mid- and Long-Term Results of Larrad Biliopancreatic Diversion. Obes Surg. 2007; 17: 202-210. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17476873
- Guedea ME, Arribas del Amo D, Solanas JA, Marco CA, Bernadó AJ, et al. Results of bilio-pancreatic diversion after five years. Obes Surg. 2004; 14: 766-772. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15318979
- Gracia J, Martínez M, Aguilella V, Elia M, Royo P. Postoperative morbidity of biliopancreatic diversion depending on common limb length. Obes Surg. 2007; 117: 1306-1311. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18098399
- Alastrué A, M Rull, D Casas. Gastroplastia vertical anillada (GVA) vs bandeleta hinchable (Lapband). Cir Esp. 1996; 60: 181-187.
- Scott HW. A tribute to Edward E Mason. The 1st Annual Edward E. Mason Founders lecture. Obes Surg. 1991; 1: 13-19. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10715655
- Blommers T. The ASBS first nine years. Obes Surg. 1992; 2: 115-117.
- Mason EE, Amaral J, Cowan GS Jr, Deitel M, Gleysteen JJ, et al. Standards for reporting results. Obes Surg. 1994; 4: 56-65. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10742766
- Wittgrove A, Clark W, Tremblay L. Laparoscopic gastric bypass. Roux-en-Y. Preliminary report. Obes Surg. 2004; 4: 353–357.
- Wittgrove A, Clark W. Laparoscopic gastric bypass. Roux-en Y. Experience with 27 cases with 3-18 months follow up. Obes Surg. 2006; 6: 54–57. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10731251
- Wittgrove A, Clark W, Schubert K. Laparoscopic gastric bypass. Roux-en Y. Technique and results in 75 patients with 3-30 months follow up. Obes Surg. 2006; 6: 500–504. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10729899
- Wittgrove A. Laparoscopic gastric bypass. Circular stapler technique. In: Obesity Surgery: Principles and Practice. Pitombo C, Jones KB, Higa KD, Pareja JC). Albany, New York: McGraw Hill Medical. 2007; 221-224.
- Baltasar A, Bou R, Miró J, Serra C. Bypass gástrico por laparoscopia. Cir Esp. 2000; 67: 556–559.
- Baltasar A, Bou R, Bengochea M. Lap Roux-Y gastric bypass. V-18. Obes Surg. 1998; 8: 393.
- Serra C, Baltasar A, Bou R, Miró J, Cipagauta LA. Internal hernias and gastric perforation after laparoscopic gastric bypass. Obes Surg. 1999; 9: 546-549. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10638480
- Higa K, Boone K, Ho T. Complications of the Laparoscopic Roux-en-Y Gastric Bypass: 1,040 Patients - What Have We Learned? Obes Surg. 2000; 10: 509-513. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11175957
- Baltasar A. Obesidad y cirugía. Cómo dejar de ser obeso. Libro de Editorial Arán. 2000.
- Martínez C. Martínez G. Bypass gástrico laparoscópico. Vitoria. 2001.
- De la Cruz F, la Cruz JL. Laparoscopic Gastric Bypass. Obes Surg. 2006; 16: 112.
- García Caballero M, Tinahones F, Cohen R. Cirugía de la diabetes mellitus tipo 2: el gran descubrimiento de la cirugía bariátrica. Nutr Hosp. 2010; 25: 693-694.
- Gumbs AA, Gagner M, Dakin G, Pomp A. Biliopancreatic diversion with a duodenal switch. Obes Surg. 1988; 8: 267–282. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17894158
- Marceau P, Biron S, Bourque RA, Potvin M, Hould FS, et al. Biliopancreatic Diversion with a New Type of Gastrectomy. Obes Surg. 1993; 3: 29-35. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10757900
- Baltasar A, Bou R, Marcote E. Hybrid bariatric surgery: Biliopancreatic diversion and duodenal switch. Obes Surg. 1995; 5: 419–423.
- Ren CJ, Patterson E, Gagner M. Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg. 2000; 10: 514-523. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11175958
- Alastrué A, M Rull, D Casas. Gastroplastia vertical anillada (GVA) vs bandeleta hinchable (Lapband). Cir Esp. 1996; 60: 181-187.
- Scott HW. A tribute to Edward E Mason. The 1st Annual Edward E. Mason Founders lecture. Obes Surg. 1991; 1: 13-19. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10715655
- Blommers T. The ASBS first nine years. Obes Surg. 1992; 2: 115-117.
- Mason E, Amaral J, Cowan G, Deitel E, Gleysteen JJ, et al. Standards for reporting results. Obes Surg. 1994; 4: 56-65. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10742766
- Wittgrove A, Clark W, Tremblay L. Laparoscopic gastric bypass. Roux-en-Y. Preliminary report. Obes Surg. 2004; 4: 353–357.
- Wittgrove A, Clark W. Laparoscopic gastric bypass. Roux-en Y. Experience with 27 cases with 3-18 months follow up. Obes Surg. 2006; 6: 54–57. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10731251
- Wittgrove A, Clark W, Schubert K. Laparoscopic gastric bypass. Roux-en Y. Technique and results in 75 patients with 3-30 months follow up. Obes Surg. 2006; 6: 500–504. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10729899
- Wittgrove A. Chapter 21: Laparoscopic gastric bypass. Circular stapler technique. In: Obesity Surgery: Principles and Practice. Pitombo C, Jones KB, Higa KD, Pareja JC). Albany, New York: McGraw Hill Medical. 2007; 221-224.
- Baltasar A, Bou R, Miró J, Serra C. Bypass gástrico por laparoscopia. Cir Esp. 2000; 67: 556–559.
- Baltasar A, Bou R, Bengochea M. Lap Roux-Y gastric bypass. V-18. Obes Surg. 1998; 8: 393.
- Serra C, Baltasar A, Bou R, Miró J, Cipagauta LA. Internal hernias and gastric perforation after laparoscopic gastric bypass. Obes Surg. 1999; 9: 546-549. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10638480
- Higa K, Boone K, Ho T. Complications of the Laparoscopic Roux-en-Y Gastric Bypass: 1,040 Patients - What Have We Learned? Obes Surg. 2000; 10: 509-513. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11175957
- Baltasar A. Obesidad y cirugía. Cómo dejar de ser obeso. Libro de Editorial Arán. 2000.
- Martínez C. Martínez G. Bypass gástrico laparoscópico. Vitoria. 2001.
- De la Cruz F, la Cruz JL. Baipás Gástrico por Laparoscopia. Laparoscopic Gastric Bypass. Obes Surg. 2006; 16: 112.
- García Caballero M, Tinahones F, Cohen R. Cirugía de la diabetes mellitus tipo 2: el gran descubrimiento de la cirugía bariátrica. Nutr Hosp. 2010; 25: 693-694.
- Hess DS, Hess DW. Biliopancreatic diversion with a duodenal switch. Obes Surg. 1988; 8: 267–282.
- Marceau P, Biron S, Bourque RA, Potvin M, Hould FS, et al. Biliopancreatic Diversion with a New Type of Gastrectomy. Obes Surg. 1993; 3: 29-35. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/10757900
- Baltasar A, Bou R, Marcote E. Hybrid bariatric surgery: Biliopancreatic diversion and duodenal switch. Obes Surg. 1995; 5: 419–423.
- Ren CJ, Patterson E, Gagner M. Early results of laparoscopic biliopancreatic diversion with duodenal switch: a case series of 40 consecutive patients. Obes Surg. 2000; 10: 514-523. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11175958
- Baltasar A, Bou R, Miró J. Avances en técnica quirúrgica. Cruce duodenal por laparoscopia en el tratamiento de la obesidad mórbida: técnica y estudio preliminar. Cir Esp. 2001; 70: 102-104.
- Baltasar A, Pérez N, Bou R. A switch to the Duodenal Switch. Glob J Obes Diabetes Metab Syndr. 2019; 6: 001-009.
- Baltasar A, Bou R, Pérez R, Serra C, Bengochea M. Twenty-five years of duodenal switch. How to switch to the duodenal switch. Nutr Hosp. 2019; 36: 1278-1287. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/31657604
- Serra C, Pérez N, Bou R, Baltasar A. Sliding Self-Locking First Stitch and Aberdeen Knots in Suture Reinforcement with Omentoplasty of the Laparoscopic Gastric Sleeve Staple line. Obes Surg. 2014; 24: 1739–1740.
- Baltasar A, Bou R, Serra R, Bengochea M, Pérez N. Use of self-locking knots in running intestinal bariatric sutures. Glob Surg. 2015; 2: 100-101.
- Baltasar A, Bou R, Serra C, Bengochea M, Pérez N. Self-Locking Sliding Knots in Laparoscopic Bariatric Sutures Baltasar A, Self-Locking Sliding Knots in Laparoscopic Bariatric Sutures. Clinics Surg. 2020; 2: 1-2.
- Recomendaciones de la SECO para la práctica de la cirugía bariátrica (Declaración de Salamanca). Cir Esp 2004; 75: 312-314.
- Baltasar A, Serra C, Pérez N, Bou R, Bengochea M, et al. Laparoscopic sleeve gastrectomy. A multi-purpose operation. Obes Surg. 2005; 15: 1124–1128. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16197783
- Ahmad SS, Ahmad SS, Kohl S, Ahmad S, Ahmed AR. The Hundred Most Cited Articles in Bariatric Surgery. Obes Surg. 2015; 25: 900–909. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25720513
- Angrisani L, Santonicola A, Iovino P, Vitiello A, Higa K, et al. IFSO Worldwide Survey 2016: Primary, Endoluminal, and Revisional Procedures. Obes Surg. 2018; 28: 3783–3794. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30121858
- Rutledge R. The Mini-Gastric Bypass: Experience with the First 1,274 Cases. Obes Surg. 2001; 11: 276-280. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11433900
- Carbajo M, García-Caballero M, Toledano M, Osorio D, García-Lanza C, et al. One anastomosis gastric bypass by laparoscopy: results of the first 209 patients. Obes Surg. 2004; 15: 398-404. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15826476
- Sánchez-Pernaute A, Rubio Herrera MA, Pérez-Aguirre E, García Pérez JC, Cabrerizo L, et al: Proximal Duodenal–Ileal End-to-Side Bypass with Sleeve Gastrectomy: Proposed Technique. Obes Surg. 2007; 17: 1614–1618. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18040751
- European Centers of Excellence for bariatric surgery. Baltasar A. Editorial. BMI. 2011; 1: 1.
- Baltasar A, Bou R, Miró M, Bengochea M, Pérez N. V13. Hand-sutured laparoscopic duodenal switch: technical aspects. IFSO-2002-Sao Paulo. Obes Surg. 2002; 12: 455.
- Baltasar A. Historical note: First diabetes metabolic operation in Spain. Integr Obes Diabetes. 2015.
- Resa J, Solano J, Fatás A, Blas JL, Monzón A, et al. Laparoscopic Biliopancreatic Diversion: Technical Aspects and Results of our Protocol. Obes Surg. 2004; 14: 329-333. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/15072652
- Resa J, Lagos J, Pérez A. Laparoscopic Gastro ileal Bypass with Single Anastomosis: Analysis of the First 1512 Patients. Laparoscopic Gastroileal Bypass with Single Anastomosis. Obes Surg. 2019.
- Alhambra M, Molina M, Prior M, Manzano-García G, Calañas-Continente A, et al Variations in diabetes remission rates after bariatric surgery in Spanish adults according to the use of different diagnostic criteria for diabetes. BMC Endocr Disord. 2017; 17: 51. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/28810850
- Vidal J, Ibarzabal A, Romero F, Delgado S, Momblán D, et al. Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects. Obes Surg. 2008; 18: 1077-1082. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18521701
- Vilarrasa N, Rubio MA, Miñambres I, Flores L, Caixàs A, et al. Long-term outcomes in patients with morbid obesity and Type 1 Diabetes Undergoing Bariatric Surgery. Obes Surg. 2017; 27: 856–863. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27709487
- García M, Tinahones FG, Cohen R. McGraw-Hill Interamericana de España S.L.1ª ed., 1ª imp. 2011.
- Cruz M, Rubio MA, Calle L. Remisión de diabetes mellitus tipo 2 a largo plazo tras cirugía bariátrica Tesis. Hospital Clínico. 2017.
- Torres A, Sánchez A, Rubio MA. Metabolic surgery for obesity a critical account. Endocrinol Nutr. 2013; 60: 36-38. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24490225
- Baltasar A, Serra C, Bou R, Bengochea M, Andreo L. Sleeve Gastrectomy in a 10-year-old Child. Obes Surg. 2008; 18: 733–736. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/18401672
- Baltasar A. Nine years follow up of the 1st Adolescent Bariatric Surgery in Spain Nine years follow up of the 1st Adolescent Bariatric Surgery in Spain. J Obes. 2017; 3: 026.
- Carbajo M, Vázquez R, Aparicio R, Luque de Leon E, Jimenez JM, et al. 12-year old adolescent with super morbid obesity, treated with laparoscopic one anastomosis gastric bypass (LOAGB/BAGUA): A case report after 5-year follow-up. Nutr Hosp. 2015; 31: 2327-2332. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/25929410
- Carbajo MA, González G, Jiménez JM, Luque-de-Leon E, Ortiz-de-Solorzano J, et al. A 5-Year Follow-up in Children and Adolescents Undergoing One-Anastomosis Gastric Bypass (OAGB) at a European IFSO Excellence Center (EAC-BS). Obes Surg. 2019; 29: 2739-2744. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/31049849
- Vilallonga R, Moreno JM, Yeste D, Sánchez Santos R, Casanueva Freijo F, et al. Initial Approach to Childhood Obesity in Spain. A Multisociety Expert Panel Assessment. Obes Surg. 2017; 27: 997–1006. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/27752806
- Vilallonga R, Fort JM, Caubet E, González O, Armengol M. Robotic Sleeve Gastrectomy Versus Laparoscopic Sleeve Gastrectomy: a Comparative Study with 200 Patients. Obes Surg. 2013; 23:1501–1507. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/23897216
- Morales S. Bypass gástrico por puerto único: detalles técnicos. De un nuevo abordaje. Cir Es. 2015; 90: 100-106.
- Morales-Conde S, Peeters A, Meyer YM, Antoniou SA, Del Agua IA, et al. European association for endoscopic surgery (EAES) consensus statement on single-incision endoscopic surgery. Surg Endosc. 2019; 33: 996-1019. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/30771069
- Shikora S, Torres A. Baltasar. biography. Obes Surg. 2016; 26: 477–478.
- Rafael Álvarez Cordero. Biography. Obes Surg. 2016; 26: 1997–1998.
- Torres AJ. Biography. Obes Surg. 2017; 27: 2383-2384.
- Baltasar A. Rafael Capella biography. Obes Surg. 2017; 27: 1129.
- Baltasar A, Luque-de-León E, Carbajo MA. Carbajo biography. Obes Surg. 2018; 28: 889–891.
- Gastrectomía vertical laparoscópica. Wikipedia GVL.
- Wikipedia en CD.
- Baltasar A, Bou R, Bengochea M, Serra C. Malnutrición calórico-proteica. Tres tipos de alargamiento de asa común. BMI-Latina. 2011; 5: 96-97.
- Baltasar A, Bou R, Bengochea M. Fatal perforations in laparoscopic bowel lengthening operations for malnutrition. Surg Obes Relat Dis. 2010; 6: 572–574. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/20176511
- Bueno J, Pérez N, Serra C. Fistula pancreato-cutánea secundaria a pancreatitis postoperatoria tras cruce duodenal laparoscópico. Cir Esp. 2004; 76: 184–186.
- Serra C, Baltasar A, Andreo L, Pérez N, Bou R, et al. Treatment of Gastric Leaks with Coated Self-expanding Stents after Sleeve Gastrectomy. Obes Surg. 2007; 17: 866-872. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/17894143
- Serra C, Baltasar A, Pérez N, Bou R, Bengochea M. Total Gastrectomy for Complications of the Duodenal Switch, with Reversal. Obes Surg. 2006; 16: 1082-1086. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/16901364
- Castillo J, Fábrega F, Escalante C, Sanjuan JC, Herrera L, et al. Liver Transplantation in a Case of Steatohepatitis and Subacute Hepatic Failure after Biliopancreatic Diversion for Morbid Obesity. Obes Surg. 2001; 11: 640–642. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/11594111
- Baltasar A. Liver failure and transplantation after duodenal switch. Surg Obes Relat Dis. 2014; 10: c93-c96. PubMed: https://www.ncbi.nlm.nih.gov/pubmed/24916757
- Mayo MA, Pacheco JM, Pérez D. Caso clínico Fallo hepático fulminante a largo plazo en pacientes sometidos a baipás gástrico por obesidad mórbida. Nutr Hosp. 2015; 32: 430-434.
- Baltasar A, Bou R, Serra C. Grapado de la sonda en gastrectomía vertical laparoscópica. BMI-latina. 2013; 3: 4-7.
- Baltasar A, Bou R, Bengochea M. Intubación Difícil y Traqueotomía en el obeso mórbido Baltasar A.: BMI. 2013; 3: 4.
- Baltasar A. Prevenir y Deshacer entuertos en cirugía. Jo Negative Non-Positive Results. 2019; 4: 252-264.
- Duncan T, Tuggle K, Larry Hobson L. PL-107. Feasibility of laparoscopic gastric bypass performed on an outpatient basis. Surg Obes Relat Dis. 2011; 7: 339–354.