More Information
Submitted: 20 February 2020 | Approved: 26 March 2020 | Published: 27 March 2020
How to cite this article: Motwani M, Palvia R, Nanda B, Motwani M, Chaubal B, et al, ECHO…for a change!!. New Insights Obes Gene Beyond. 2020; 4: 001-003.
DOI: 10.29328/journal.niogb.1001011
Copyright License: © 2020 Motwani M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
ECHO…for a change!!
Manish Motwani*, Rajeev Palvia, Bhavesh Nanda, Mahek Motwani, Bhakti Chaubal, Jyoti Kesarkar, Bhakti Mange and Sneha Shukla
Department of Bariatric Surgery, Aastha Health Care, Maharashtra, India
*Address for Correspondence: Dr. Manish Motwani, Bariatric Surgeon and Programme Director, Department of Bariatric Surgery, Aastha Bariatrics, Aastha Health Care, Mulund, Mumbai, Maharashtra, India, Email: [email protected]
The childhood obesity is increased more than three folds in last two decades in developed world. There is nutritional transition seen in the developing world including India. The westernization in diet of the Indian population along with prosperity brings the brunt of overweight and obesity. This has future implications of liver diseases, heart diseases, hypertension, hyperlipidaemia, insulin resistance; malignancies. Mumbai is the prosperous city and an economical capital of India. Also, the rampant use junk food, common outdoor eating’s, no grounds to play for children make the high likelihood that the prevalence of obesity to be higher than rest of the country.
It can profoundly affect children’s physical health, social, and emotional well-being and self-esteem. It is also associated with poor academic performance and a lower quality of life experienced by the child.
One of the best strategies to reduce childhood obesity is to improve the eating and exercise habits of the entire family. Treating and preventing childhood obesity helps protect the child’s health and has tremendous impact on child’s Physical and academic performance.
And hence we at Aastha Bariatrics took initiative and launched ECHO... for a change (‘E’radicating ‘C’Hild ‘H’ood ‘O’besity), a pan Mumbai campaign against childhood obesity.
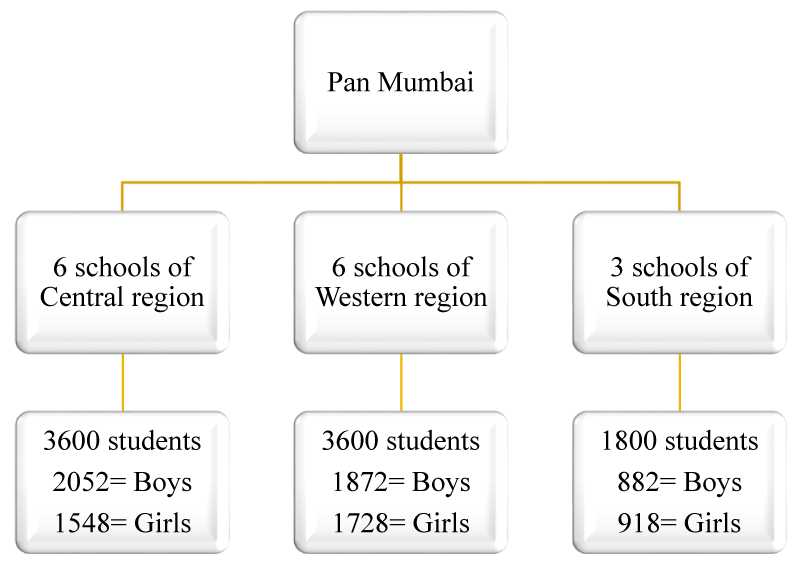
This campaign was done in 15 high schools across Mumbai, which covered in total of 9000 students.
Body composition analysis
This cross-sectional study carried out for 3 months. The permission from the principal, parents and assent from the students were taken prior the screening.
This study incorporated primary analysis of anthropometric measurements (Height, weight, BMI, body fat) of total 9000 children in the age group of 11 to 15 years, studying in class 6th to 9th standard, from all 3 regions of Mumbai i.e. Central region from Thane to Dadar, Western region from Andheri to Bandra, and South region from Chhatrapati Shivaji Maharaj Terminus to Dadar (Table 1).
Table 1: Flow chart for sample covered from 3 regions of Mumbai.
BMI percentile for children are:
Children were categorized into three groups: obese (> 95th percentile), overweight (≥ 85th percentile) and normal (< 85th percentile, > 5th percentile) using age- and sex-specific percentiles of BMI.
The prevalence of overweight and obesity were calculated by calibrated scales and using BMI for age/gender percentiles derived through child and teen BMI calculator developed by CDC. Structured questionnaires were designed for detailed diet recalls, assessment of physical activity patterns. Data collection was done by nutritionist with assistance of two trained interns.
Nutrition assessment
Detailed diet recall questionnaire was circulated to each and every student. Interaction with parents and teachers were done regarding the food patterns, school lunches, snacking patterns, family eating habits, outings, their likes and dislikes were studied in detail.
Students were asked to fill 24-hour diet recall form and submit it to their respective class teachers
Habitual activity assessment
The physical activity pattern was assessed through interaction with parents and teachers both. Child’s socialising, active participation in curriculum was discussed with parents and teachers. Even the frequency of screening time i.e the time children are spending on TV/laptop/mobile phones and time for outdoor activity were noted down with the help of structured questionnaire.
Physical evaluation
Each student was evaluated for any present medical conditions and physical appearance like:
• Breathlessness
• Lethargy
• Double chin
• Excessive sweating
• Tiredness after even little activity
• Dark patches around neck
• Excess weight in abdomen and waist
Data of around 9000 students was collected from 15 schools across Mumbai, out of which 53.4% (4806) were boys and 46.6% (4194) were girls.
Table 2 shows, out of 4806 male students, 1028 (21.6%) were overweight and 817 (16.8%) were obese [BMI between 85th-95th percentile and > 95th percentile respectively]. Whereas out of 4194 female students, 805 (18.8%) were overweight and 612 (14.3%) were obese.
| Table 2: Gender wise distribution of Body Mass Index.cc | ||||||||
| Central region | Western region | South region | Total | |||||
| BMI | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls |
| Overweight (85th -95th percentile) | 437 | 297 | 389 | 352 | 202 | 156 | 1028 | 805 |
| Percentage | 21.3% | 19.2% | 20.8% | 20.3% | 22.9% | 17% | 21.6% | 18.8% |
| Obese (>95th percentile) | 339 | 251 | 337 | 247 | 141 | 114 | 817 | 612 |
| Percentage | 16.5% | 16.2% | 18% | 14.3% | 16% | 12.40% | 16.8% | 14.3% |
At the time of dietary evaluation, it’s been observed that out of 9000 students, 3537 (39.3%) students were vegetarian and 5463 (60.7%) students were non vegetarian.
The frequency of junk food was also analysed through the detailed 24-hour diet recall which was filled in by parents. In this form parents were asked to mention the frequency of outside/junk food, snacking pattern, and snack preferences of their children (Table 3).
| Table 3: Frequency of Junk food. | ||
| Frequency of junk food | Boys (4806) | Girls (4194) |
| Daily | 217 (4.5%) | 130 (3.1%) |
| Once a week | 1778 (37%) | 1367 (32.6%) |
| More than once a week | 2076 (43.2%) | 1598 (38.1%) |
| Occasionally | 735 (15.3%) | 1099 (26.2%) |
When the parents and students were interrogated regarding the daily routine of them, it was found out that the number of children spending time in front of TV/laptop/mobile phones for more than 2 hours a day was 5337 (59.3%), whereas number for less than 2 hours a day was 3663 (40.7%).
Clinical assessment of overweight/obese students
The students whose BMI was above 85th percentile were assessed thoroughly for any preexisting health issues and the findings were: (Table 4).
| Table 4: Clinical assessments and presence of medical issues of overweight/obesity | ||||
| Medical Conditions | Overweight | Obese | ||
| Boys (n = 1028) | Girls (n = 805) | Boys (n = 817) | Girls (n = 612) | |
| Breathlessness | 223(21.6%) | 167(20.8%) | 402 (49.2%) | 314(51.3%) |
| Lethargy | 390(37.9%) | 216(26.8%) | 591 (72.3%) | 420(68.7%) |
| Double chin | 426(41.4%) | 306(38%) | 760(96%) | 548(89.6%) |
| Excessive Sweating | 188 (18.3%) | 162(20.1%) | 397(48.6%) | 314(51.3%) |
| Dark patches around neck | 136(13.2%) | 88 (10.9%) | 380(46.5%) | 239(39%) |
| Excess weight around abdomen and waist | 480(46.7%) | 388 (48.2%) | 770(94.2%) | 572(93.4%) |
| Depression/anxiety | 94(9.2%) | 101 (12.6%) | 215(26.3%) | 225(36.8%) |
After analysing the entire data, the parents- teacher education program was held where both the parents and teachers have been educated for home- based and school- based interventions to improve the health and to prevent further complications in child’s life. Few examples are as follow:
School-based interventions
High importance on physical activity
• Making healthier choice available and banning un-healthy food in cafeteria, (sweetened beverages and energy-dense junk food). Teachers can play a vital role in this initiative
• Training of teachers regarding nutrition education
• Incorporation of more knowledge about nutrition and physical activity and nutrition related diseases in school curriculum
Home-based interventions
• Key goals to address are the common diet-related problems encountered in children, set firm limits on television and other media early in the child’s life, and establish habits of frequent physical activity
• TV/computer time to be restricted to maximum 1 h/day
• Mandatory 60 min of physical activity daily to be supervised by parents
• Restriction on eating out at weekends and restricting availability of junk foods at home
• Keep healthy snacks at home which can be easily accessible to the child
Parents were provided with many easy and healthy eating options for their children. One to one counselling was also conducted for the parents whose children were fallen under overweight/obese category. Teachers were advised to implement more outdoor/fitness activities and to motivate students for active participation, random checking of lunch boxes, organising more health/fitness program to improve their knowledge regarding healthy foods and lifestyle.
All the schools will be approached after 6 months to reanalyse the data to observe the results of implementation of effective interventions.